According to the Institute of Healthcare Improvement (IHI), up to 50 percent of all medication errors and up to 20 percent of adverse drug events (ADEs) in the hospital occur as a result of “inconsistent knowledge and record keeping about medications.”In response, the IHI has defined a three-step medical reconciliation process of verification, clarification, and reconciliation, and this is typically the standard of care in all hospitals. But, although 2014 is the tenth year that medication reconciliation has been part of the Joint Commission’s National Patient Safety Goal, there is still much work to be done.
To truly move the pharmacy practice forward and make medication errors and ADEs things of the past, hospital leaders must enhance the medication verification process. According to Bradley L. McNew, PharmD, of the Clinical Workflow Improvement Department at the BJC Learning Institute in St. Louis, MO, there are several steps that administration can take to ensure that their operations don’t just meet the National Patient Safety Goal for medication reconciliation, but exceeds it.
Some possible actions that the C-suite can take include common-sense solutions such as collecting accurate medication histories upon admission. One St. Louis hospital had encountered the problem of patients not remembering their medication histories—in response, the facility implemented an automated system that, with patient consent, collects medication histories from retail pharmacy databases to provide an accurate picture of all medications that patient has ever purchased using insurance.
While pharmacist-led medication counseling and interviews have been widely recommended by pharmacy organizations in recent years, another potential solution to lax reconciliation procedures is involving pharmacists themselves—not just pharmacy technicians and nurses—in a computer-assisted medication verification process.
However, this solution isn’t always practical—budgetary constraints can often prevent the pharmacist from becoming a full-on participant in the clinical team.
But McNew proposes a reasonable compromise: “While hospital administrators may object to paying a pharmacist to perform medication verification and to be involved in all stages of the medication reconciliation process, i’s imperative to weigh the cost of the pharmacist against the potential costs of ADEs and decreased reimbursement due to readmissions—not to mention the cost of patient harm due to ADEs.”
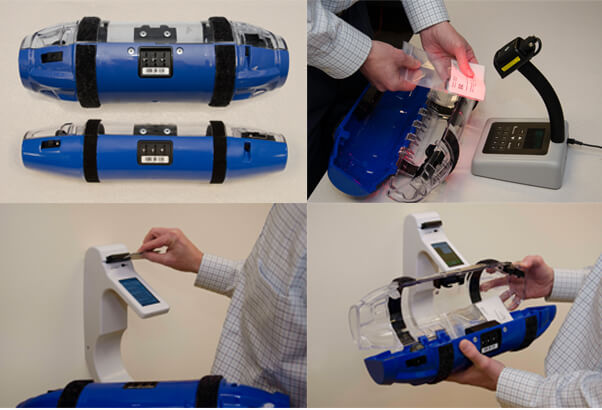
 By implementing a patient safety safeguard like Aethon’s patented TUG autonomous robots, MedEx medication tracking, or the TubeTrack secured and traceable pneumatic tube solution, hospitals achieve two important goals leading to increased pharmacy team involvement in the continuum of care:
By implementing a patient safety safeguard like Aethon’s patented TUG autonomous robots, MedEx medication tracking, or the TubeTrack secured and traceable pneumatic tube solution, hospitals achieve two important goals leading to increased pharmacy team involvement in the continuum of care:
- They directly reduce interruptions and distractions in the pharmacy which are known to sap the productivity of pharmacy staff, as illustrated by this publication in Patient Quality and Safety. By tracking and controlling medication delivery a major source of distracting phone calls is eliminated. By eliminating this non-productive time pharmacists can be available for more productive clinical activities.
- These systems, among other security measures, employ scannable barcodes and locking mechanisms that ensure that all medications can be tracked to their clinical hand-off point. This means hospitals can eliminate the logistical headache of confirming, verifying, and tracking medications, without the need to hire additional personnel. And this allows your pharmacists to do what they do best, while providing exceptionally efficient, accurate patient care.
